Insights + interviews
In Conversation with Dr. Snehal Patel and Dr. Vas Metupalle
The Active Age had a chat with Dr. Snehal Patel and Dr. Vas Metupalle, executives at MyDoc, an integrated healthcare platform that merges record-keeping functions into one easy-to-use tool for healthcare organisations.
e-health is gaining popularity due to increased demand for internet-enabled, mobile-friendly health services, an aging population and increasing smartphone penetration. A 2014 Mckinsey report shared that up to 75 percent of Southeast Asia healthcare customers want to be provided with digital health services.
The healthcare industry – patients, doctors, employers and insurers – aim to reduce costs by focusing on prevention and early intervention. However, the healthcare system is generally struggling with information management, storage and referrals. Health records and data tend to be silo-ed, or lost, making it difficult to get a complete picture of the patient’s health.
Dr. Patel and Dr. Metupalle founded MyDoc to unify fragmented data, and provide patients and healthcare providers with a secure system for communications and care management.
With the MyDoc system in place, patients can receive low-level, non-intrusive monitoring. This can help lighten healthcare providers’ workloads and saves transportation time and costs for patients.
In a nutshell, for less overall cost, patients gain greater access to necessary care through more continuous disease management. Health issue developments are reported earlier and corrective action can be taken sooner, preventing the escalation of disease.
Preventive and chronic disease management is dependent on the smooth transition of referrals and multiple provider care, that the MyDoc platform provides. Patients with chronic diseases and conditions requiring several healthcare providers will especially benefit from consistent monitoring as MyDoc can link GPs, specialists and hospitals together.
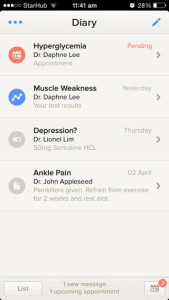
MyDoc is currently the first digital health startup to partner with Guardian Pharmacy to bring healthcare directly to customers. Through an in-store device and on the Guardian Pharmacy website, customers can have video consultations and chat securely with certified healthcare professionals. The system also integrates a private health diary feature that enables customers to store their health information.
MyDoc is currently available on the iOS and Android operating systems and also accessible through a web browser. The company works with clinics, general practitioner (GP) hospitals and healthcare provider networks.

The Active Age (TAA): What’s the objective behind a platform such as MyDoc?
Dr. Patel (DP): As people age, some people are going to have chronic diseases, others issues become more paramount, and the way to manage them is very important.
And I think the objective behind MyDoc is to make the management simpler, easier to obtain, and to allow those people to spend more time doing other things with their lives, as opposed to focusing on the issue.
We look at a business-to-business-to-consumer (B2B2C) model because we believe in empowering the ecosystem. There’s a lot of very good resources available to aging persons in Singapore. We just want to make the access points more convenient and much more robust.
TAA: Can you give us some highlights about the partnership with Guardian? You shared that some customers are really good at asking questions already, directing clinical questions to the doctor and other questions to the pharmacists.
DP: The partnership with Guardian started off from their E-Commerce programme, where they could make the provision of products easier to access for the consumers. We realised that, particularly for the health market, even for health products, consumers tend to have less information, when they want to purchase products that are not easily understood.
When you buy from Amazon or any local E-Commerce portal, consumers already know they want to buy a specific item or quantity; there isn’t much for decision making. However, when it comes to health, there’s a lot of information symmetry. People tend to be more skeptical, they are always concerned about buying the right medication, buying the right dosage for my son, my child, for my grandchild.
The service we provide is really to make it easy for the average consumer to gain access to those services. They won’t have to go down to the mall, or to the store, they just wait for the products to come to them. And they will have the confidence that they bought the right products because they have spoken to the pharmacist or doctor.
Dr. Metupalle (DM): We basically have two sides of our product. One is the professional component, where we help the service providers improve productivity in terms of providing care.
Consumers and patients can also benefit by accessing their own personal MyDoc account. We improve productivity across the service providers who care for them. For example, they can be nurses handling home care or coming to take blood from your home, the lab assistants that will push the results to MyDoc. So there is care coordination done.
TAA: MyDoc seems to serve as a bridge to the patient across different service providers. Walk me through this scenario. I have a primary caregiver, most likely a family member. As a caregiver, I will be getting a lot of updates, for example, blood test resultings coming in. Will the nurse or healthcare person updating be from my medical provider or a third-party MyDoc service provider?
DM: We partner with several organisations. One of them you mentioned is Guardian. Similarly, we work with other medical groups such as primary care groups to bring GPs online. There are also healthcare groups and nursing groups that are already on MyDoc. We are able to tap on them to provide services to our consumers.
TAA: If a consumer signs on with MyDoc, do they still need to have another service agreement with the third party service provider to access services?
DM: So if it’s a consumer, there’s no agreement. If you walk into a GP, they don’t have an agreement with their patients. It’s whether they want to consume those services.
MyDoc is not a shopping site. We work with the medical groups that want to use our platform and to make it easier for them to serve a wide pool of the community. For consumers and patients, it’s easier for them to access these medical groups directly. We are a software platform available on mobile and web.
We help provide an experience of convenient access from the consumer to the healthcare providers.
TAA: So it’s a service provider that I already have. For example, I have diabetes, so someone advises me on when I take my insulin jabs. The service provider pairs with My Doc, and that’s when I can access my medical record through a browser at home, direct from my doctor who tells me about the report.
DP: If you were to take a step back, and think about hospital settings. Typically, as a patient, you will have more points of contact with the healthcare system.
And what I mean by that is that you have a nurse, you have a GP, all sorts of specialists, consulting you at the hospital. The minute you leave the hospital and go out to an outpatient setting, you suddenly have all these different points you may need access to and no one central coordinator. No one is using the same database. No one is using the same record system. So it becomes very complicated quickly.
For the average population, many people will have a disease. However, it’s not so severe that they have to be in a hospital. They don’t need constant monitoring, constant engagement. But this is a particular problem when you are going to five different doctors, in four different places, and no one using the same medical record systems, so what we are trying to do is to make that much simpler.
So in other words, if you are on MyDoc and perhaps you have high-blood pressure, diabetes and hypertension. That person is seeing a GP for most of the conditions, but he’s also seeing a cardiologist or another specialist as well. Assuming all three providers are on MyDoc, it becomes very easy for the GP to provide care for the patient, whether it’s high-blood pressure or the diabetes.
That’s actually very important, because if you are the primary caregiver for that person, you need to know what else is going on and right now, the system is very fragmented so they don’t have that.
With MyDoc, the GP or primary caregiver is empowered, they look at data and information, and often times the patient does not have to come into the clinic. Obviously, the patient saves a tremendous amount of time in the sense that there is no queuing, no car visits, no buses. Patients can be given a much better level of service and yet spend much less time overall.
DM: The last few years of someone’s life is when they spend most of the time in hospitals. It’s not the first twenty years of this ageing process. And that’s why they end up mostly needing this outpatient care. And outpatient care is very not coordinated, and it’s either they know one GP and they go back to the same GP. Yes, it’s a good thing if they go back to the same GP. Unfortunately, some might start going around to many different clinics.
TAA: To simplify for the reader, what happens if I am the patient and I have a GP and he tells me that my blood level goes to a certain level and he needs to talk to me about medication.
DP: MyDoc is actually is more advanced than that. Doctors want to focus on the data that can have the most impact. So our job is the curation of data. So for the scenario about high blood sugar high, the right audience is not your doctor. The right audience is a nurse sitting at the clinic.
DM: For a decision maker, the nurse has to ask the doctor if she’s not clear about certain things. And beneath a specified threshold, they can communicate about the patient.
DP: And because the nurse understands the issue. The nurse may contact you and say, if it happens again, you know to check in with the clinic.
DM: With MyDoc, the nurse can do a direct peer-to-peer connection between the patient and the doctor. It’s a direct consult, basically. We have video in our system, but messaging is the most commonly used.
DP: We know how we can manage certain conditions. And what we are trying to do is to make the system more productive and more efficient, so that the patient doesn’t have to come in to the doctor’s office or A&E to get basic information, to get basic advice for things that he can get at home.
TAA: There doesn’t seem to be a primary database for the healthcare management system at a national level. The national objective also seems to be about reduction of stress on the overall system. It’s just reducing the volume of people going back to hospital or A&E and perhaps that’s why the approach is usually from a data management point of view.
DM: We are coming from a hospital angle, where they just want to make sure that there’s some data being shared from the hospital back to the community, after discharge you are able to share it to the GP.
DP: I think that’s a great point. MOH has done a very great job here in Singapore. It doesn’t have to be so complex. I don’t need to see the entire life history of medical data on my smart phone. What I need to focus on is the classic 80:20 rule.
20 percent of the patient’s history causes 80 percent of the problems. That’s very dynamic. And it turns out that I can solve 80 percent of my healthcare needs with just 20 percent of data. The trends are a very basic thing. If I can connect my GP to my specialist, that’s one. Second, if I can get my laboratory results, which there are tons of outpatient laboratories which do a very great job in monitoring glucose levels or hemoglobin, BMI or hypertension, and finally patient information.
If we just focus on these three outlets, and we do a very good job in making it very easy for both the providers and the patients to get access to that information, we solve the majority of the problems. This is not about finding solutions for 100 percent of the people. There are very sick people that need to be in hospital, and when they go out of the hospital they need to be on very complex machines that monitor their bodies. We are not that platform. We are the platform for 90 percent of the people who are active agers, who just have a couple of health issues.
DM: Or they have an annual health checkup, and they get a couple of results which they don’t understand what it means, and they want to ask questions.
TAA: Let’s shift tangent a little bit and talk about Smart Nation. How do we see a solution like My Doc being integrated into the whole smart nation environment?
DM: We are very encouraged by the kind of forward-looking approach by the Smart Nation Committee. We were at the recent IDA event on Smart Nation where I think more than half the speech was on healthcare.
DP: Yes, it was very much on healthcare and some points about driverless cars and transportation. It was very encouraging.
DM: An interesting area is telemedicine that we can divide it into a few pieces. One is tele-consultation, which is professional to patient consultation, and there’s tele-monitoring. I think that’s where you can have Internet of Things (IoT) devices, sensors, things like that. And this monitoring, although it’s early days, some data is already out there where Singapore might lead in getting data.
It may not reach everyone in the next few years yet, it will take longer than that, so we might have to be ready for it, but there’s a gradual process to it. And there’s where we fit in, to try and get real people to communicate with these patients, while bringing technology like IOT slowly into the picture.
TAA: Real people meaning specialists, doctors, nurses?
DM: To communicate on platforms like this, mobile help platforms, and then slowly making it more automated.
We are providing a patient diary and these sensors and other devices need a depository, they need to go in somewhere people can see and share these data. So this is where we are accepting and working with IoT device makers to provide this patient diary to them. They can pump in this sensor data and the professionals can see it on the dashboard and make sense of it.
DP: And I think that’s the key. There’s a lot of data in the device and I think there’s a lot of monitoring happening. But we feel that without our service, without real connectivity, that a device-alone approach won’t work.
TAA: Simple example, let’s look at wearables. 3 months, 90 days and it’s in the drawer, because no one knows what to do with the data. Again, I could almost see, if you guys had access to the data, and on the other hand you have to have service providers ready to make sense of it.
DP: That’s what we are trying to do. That’s exactly our platform. And not only that, but there’s the space we are trying to engage in making sense of the data.
DM: Not every piece of data is useful. A lot of it can be considered noise.
DP: Now, despite what the wearables makers want you to believe, doctors actually have enough information, and they don’t really care how many steps you walk. But we have nutritionists and dietitians as well, that are part of the platform. The dietitians want access to the number of steps.
For someone planning a programme, the GP is not necessary. We are able to take this information, and curate it such that the right person gets the right information. And that allows efficiency to occur.
TAA: I would love to see such a platform, a dietitian or a nutritionist looking at steps done, a couple of GPs monitoring high blood pressure, making sure it goes down. That is what a caregiver would like to know. Because you didn’t take your 10 thousand steps today, now let’s go out and take a walk. Caregivers are the only one who might have that kind of influence, especially family members over an older relative.
DM: The point about reminders is very important. I think it’s goes beyond caregivers. Caregivers sometimes need a break and when they go on a holiday, they would still need someone else to do it. I think there are a lot of initiatives now. How do you do this coordination? And that’s where we feel we have the last mile. We can be in the pockets and in the mobiles. And it doesn’t have to be always manual. It’s automated as well, reminders that set time and things like that.
TAA: So the alerts and notifications are primarily to the recipient of the care, or is it to the caregiver?
DM: Both. So we have email, SMS, and app notifications, according to the healthcare group and for the patient, they can receive SMS or app notifications.
TAA: So the patient can authorize the caregiver to receive it on their behalf, from their GP or to their therapists. Are there any challenges in that approval? Is it like a written letter?
DM: When you sign up with MyDoc, it means that you are approving specific permissions. Consumers and patients can either receive care from one GP, or if they decide I want to change GP, they can actually switch off the diary being shared to the first GP. Our record is very personal. The GPs have their own records. They keep their own set of clinic records. So this is from the patient’s point of view.
DP: I think the key point here is about flexibility. It’s a classic gap in the market. It’s about helping these consumers and patients access care in a way that is more convenient for them as well as for the healthcare professionals.
TAA: So why would you look to patients to request their service providers to make MyDoc available?
DP: Without MyDoc, the base case is that the patient will have the cue from all services, especially in outpatient life, they would have no simple depository for all those information.
And they would be spending a lot more of their quality time running around between appointments, trying to coordinate between different things.
We basically take all those small, fragmented groups of providers and put them together in one package. So it’s much easier for the patients.
At the end of the day, healthcare is not going to be something people want to engage in. And we should see the objective from a patient’s perspective. They want to spend as few hours in a hospital or a care facility at any time. They might want to be at the park or at the zoo with the grandchildren and not be there with the doctor.
For MyDoc, we want to make it as easy for the vast majority of people who are generally healthy, but have certain conditions, to be able to manage their own care. People like productivity and this is essentially increasing the productivity of time and improving the quality of life.