Insights + interviews
In Conversation With Senior Ophthalmologist Dr David Chan Part 2
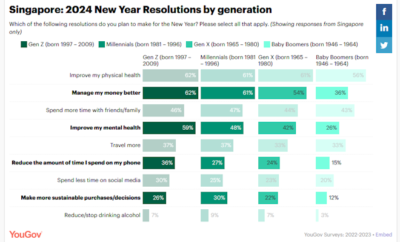
Diabetes is increasing and so is diabetic eye disease, we find out more about diabetes related eye ailments and how one can mitigate its effects.
How can diabetes affect my eyes? How does diabetes affect the retina? What are the symptoms of diabetes retina problems? These are questions commonly asked by people who suffer from diabetes. We find out more from Dr David Chan.
AA: What are some eye problems that can arise from diabetes?
DC: Diabetes is a metabolic disease that not only affects the body, it can also cause a series of eye problems known as diabetic eye disease. These conditions include diabetic retinopathy, maculopathy and macular oedema. They can cause progressive damage to the light sensitive lining at the back of the eye, known as the retina. Diabetic eye disease is a serious sight-threatening complication of diabetes.
AA: Could you tell us more in depth about diabetic retinopathy and maculopathy?
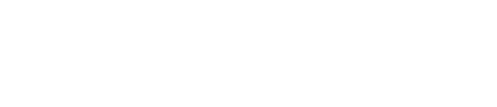
DC: Diabetic retinopathy is when there is damage to the back of the eye due to diabetes. In the earlier stages, patients have Non-Proliferative Diabetic Retinopathy (NPDR). During this stage, the blood vessels in the retina leak blood and fluid. This leakage in turn causes swelling, formation of deposits and also haemorrhages. In patients with Proliferative Diabetic Retinopathy (PDR), formation of new blood vessels occurs in an attempt to cope with the poor blood flow, which is known as neovascularisation. The new blood vessels formed are weak and fragile, and more often than not, they bleed into the clear, jelly-like substance known as the vitreous of the eye. This results in a vitreous haemorrhage, and would cause significant floaters to be seen by the patient. New blood vessels may also grow along the retina, causing scarring and pulling on the retina and eventually, retinal detachment.
AA: How about diabetic macular oedema?
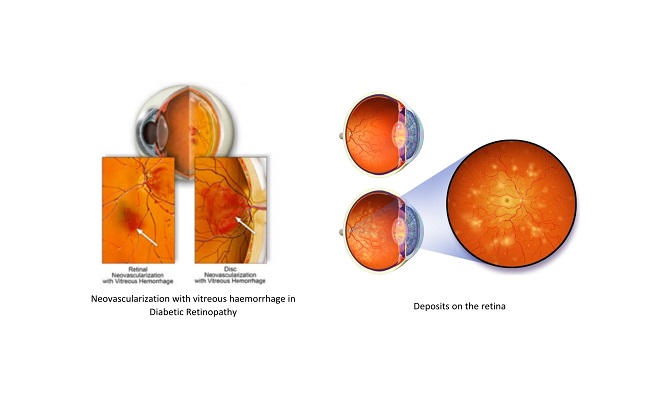
DC: Another complication of diabetes is Diabetic Maculopathy, which can present as macular oedema. Diabetic macular oedema occurs when blood vessels leak their contents into the macular region, causing it to swell. As the macular is the most sensitive part of the retina that is responsible for central vision, the swelling would cause distortion and blurring of vision. Initially, the changes to vision are not noticeable. Over time, diabetic macular oedema can cause central vision to be impaired, compromising the ability to complete day-to-day tasks such as driving, recognising faces and working. Macular oedema can occur at any stage of diabetic retinopathy. Patients with long-standing diabetes, poorly controlled blood sugars and hypertension are at higher risk of having macular oedema. If left untreated, macular oedema can lead to permanent vision loss and in serious cases, blindness.
AA: In what other ways can diabetes can affect your eyes? Would it cause problems such as the blurring of vision?
DC: Here are some potential problems to take note of if you have diabetes:
- Fluctuating vision: Patients with poorly controlled or high blood sugar levels, the shape of the lens may change due to absorption of sugar. As a result, patients will experience episodes of fluctuating or blurred vision.
- Glaucoma: New blood vessels can grow in the iris due to neovascularisation. These new vessels will cause build-up of pressure in the eyes by way of obstructing the outflow of fluid. When the pressure is high, there will be damage to the optic nerves.
- Cataract: Cataracts develop at an earlier age for patients who are afflicted with diabetes. When the sugar levels rise, the lenses swell. The high levels of glucose also affect the proteins in the eye, causing it to become less clear. This eventually leads to cataract formation, and patients would have complaints of glare or colours appearing less bright than before.
AA: What are some preventive measures to avoid these problems? Would an eye screening help?
DC: All patients with diabetes are at risk of having diabetic retinopathy. For patients who have had diabetes for many years, the chances of developing diabetic retinopathy are much higher as compared to someone who has been newly diagnosed. The progression of diabetic retinopathy is insidious and painless, and patients usually have no symptoms until vision is affected. As vision loss caused by diabetic eye disease is irreversible, it is vital to do a comprehensive dilated eye exam every six months to a year, depending on the eye health. A dilated pupil exam allows the ophthalmologist to pick up on changes in the retina such as bleeding or abnormal growth of blood vessels. Patients can do their part by staying physically active and monitoring their blood sugar levels. By doing so, the progression of diabetic eye disease would then be slowed down.
AA: Are there any treatments for the above mentioned eye problems? And how is treatment carried out?
DC: The mainstay of treatment of diabetic retinopathy is good blood sugar control. Treatment options to forestall the progress of sight threatening conditions includes the use of laser therapy to the retina that tries to prevent serious internal bleeding in the eye or inflammation and swelling of the macula. iN recent years, we have also seen the introduction of injections for the eye, either in the form of steroids or agents that prevent the formation of abnormal retinal vessels known as anti-Vascular Endothelial Growth Factor (Anti-VEGF). A healthy macula is essential for good vision. If detected early and appropriate treatment is given, the potentially serious side effects of diabetic eye disease can be managed.