The Gen XY Lifestyle
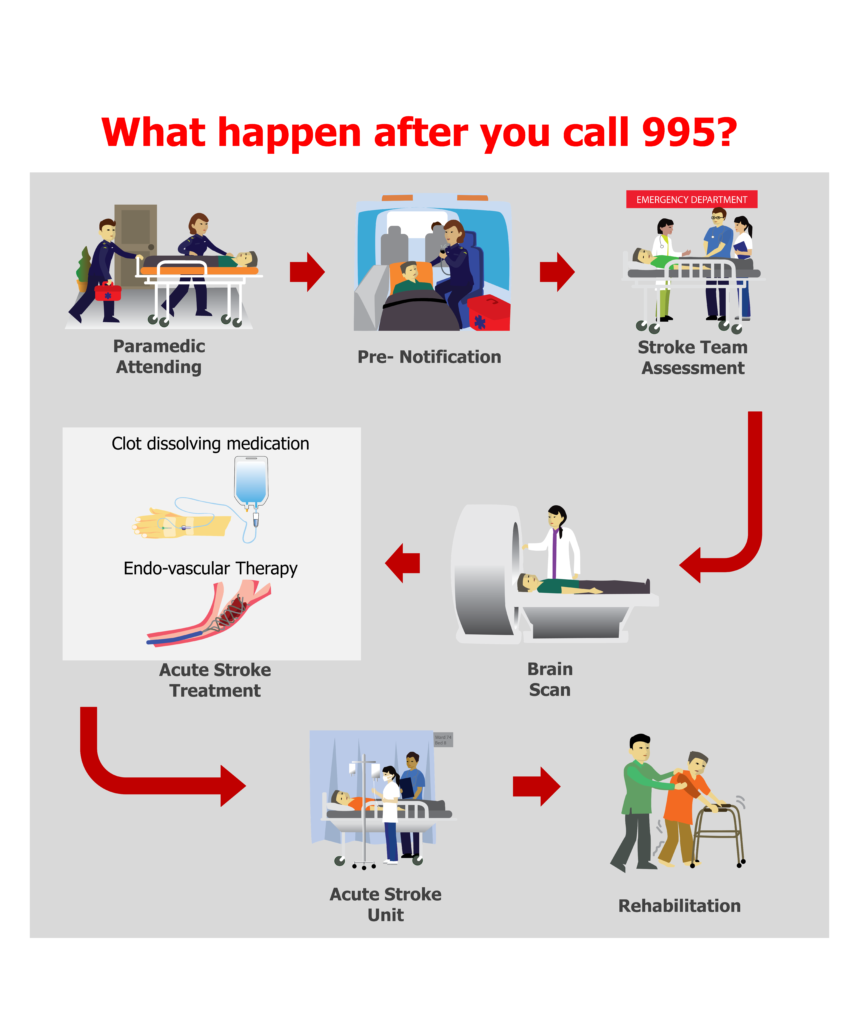
What happens after you call 995 for help with a stroke?
Stroke can have devastating consequences. It strikes suddenly and can lead to permanent disability and death. Recognition of symptoms, prompt transfer to hospital and early treatment has the potential to alter the outcome after stroke.
Act F.A.S.T. to spot stroke
Stroke is also called brain attack. There are two types of stroke ischemic (block of a blood vessel) and hemorrhagic (burst of a blood vessel). Both may present in similar way but the management of the two are different. The most common symptoms of stroke include weakness, speech disturbances, like slurring of speech/ disturbances in expression or understanding, and face drooping. Acute stroke treatments are time sensitive and have the potential to improve patient outcome. For patient to arrive the hospital in a timely manner, it is extremely crucial to recognise the common signs and symptoms of stroke, and take appropriate action immediately. This is why increasing awareness about stroke and its management in general population is important.
There is an acronym, F.A.S.T., which is devised to help people quickly spot the symptoms and warning signs of stroke by recognizing one or more of the three symptoms as described below.

Stroke is Singapore’s fourth leading cause of death and first cause of adult disability carrying significant social and economic burden. With a rapidly ageing population, the burden of stroke is expected to increase. In recent years, treatment options for acute ischemic stroke have evolved rapidly.
It is extremely important to call 995 for an ambulance.
Stroke is an emergency. Once someone suspects the possibility of stroke, time becomes very important and one should call 995 for a SCDF ambulance immediately. The ambulance paramedics are trained to assess the patient’s condition and will transfer patient to designated hospitals for further assessment and treatment. In cases of suspected stroke, the SCDF paramedics will alert the emergency department of the receiving hospital en-route so that the hospital team is ready to assess and treat the patient promptly upon arrival.
Acute stroke treatments for Ischemic Stroke
There are two types of acute ischemic stroke treatments – thrombolysis and endovascular treatment. Both treatments are time dependent and can only be administered within a critical timeframe. About 1.9 million of brain cells die every minute in the presence of impaired blood supply to brain.1
- Thrombolysis is a clot-dissolving medication administration into the blood stream by injection with aim of dissolving clot and restore blood supply to part of the brain.
- Endovascular treatment is a procedure done to remove the clot inside the blood vessel mechanically; this is performed by a specialist neuro-interventional radiologist.
Early intervention can lead to better outcome for patient
Intravenous administration of medication was first proven to be useful till three hours from stroke onset in 1995. NINDS trial showed that 13% more patients can resume all activities as pre stroke status with treatment2. Subsequently ECASS III trial showed that it is useful up to 4.5 hours from onset of stroke in patients fulfilling criteria3. This treatment carries risk of systemic bleeding, including symptomatic bleeding in brain to the extent of 6.4% in initial trial2. There is also risk of allergic reaction or angioedema which may affect breathing, thus requiring airway management.
Endovascular treatment can be done under general anaesthesia/ or sedation with local anaesthesia. During the procedure, the interventionist may use different devices like stent retrievers or suction devices to remove the clot. There were five randomised trials published in 2015 which proved efficacy of this treatment4-8. The pooled data analysis of these trials was published in 2016 which showed that with treatment 19.5% more patients achieved independent functional outcome with only some disability as compared to control9. Procedure is invasive and does carry risk of complication including but not limited to bleeding local or intracranial, vessel injury, contrast and anesthesia risk.
What to Expect in the Hospital
Upon arrival to the hospital, the patient is evaluated by the Emergency medicine doctor and the stroke team. The patient will undergo a neurological assessment and have brain scans done. These will help the stroke team to decide if the patient is suitable for acute stroke treatment. There may be patients who do not fulfil the eligibility criteria of acute stroke treatment and they will be offered other supportive treatment.
During the first few days after stroke, patients are at higher risk for recurrent stroke and complications. Therefore, stroke patients usually require admission to a hospital for monitoring, further investigation and treatment. The Acute Stroke Unit is a designated area in the hospital managed by a specialized multi-disciplinary stroke care team to deliver specialize stroke care.
The members of the stroke team may include:

Once the patient condition is stabilized, the patient will be assessed for rehabilitation needs. The patient and their family will be involved for discussion in deciding whether inpatient or outpatient rehabilitation is suitable. Upon discharge, family support and other social services play a huge supportive role in continuous improvement of patient health and reintegration into the community.
Article attributed to Dr. Prakash Paliwal, Consultant, Division of Neurology, University Medicine Cluster, National University Hospital
References:
- Saver JL. Time is brain–quantified. Stroke. 2006 Jan;37(1):263-6.
- The National Institutes of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 1995;333: 1581-1587.
- Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, Larrue V, Lees KR, Medeghri Z, Machnig T, Schneider D, von Kummer R, Wahlgren N, Toni D; ECASS Investigators. Thrombolysis with Alteplase 3 to 4.5 Hours after Acute Ischemic Stroke: N Engl J Med 2008;359: 1317-1329.
- Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, Schonewille WJ, Vos JA, Nederkoorn PJ, Wermer MJ, van Walderveen MA, Staals J, Hofmeijer J, van Oostayen JA, Lycklama à Nijeholt GJ, Boiten J, Brouwer PA, Emmer BJ, de Bruijn SF, van Dijk LC, Kappelle LJ, Lo RH, van Dijk EJ, de Vries J, de Kort PL, van Rooij WJ, van den Berg JS, van Hasselt BA, Aerden LA, Dallinga RJ, Visser MC, Bot JC, Vroomen PC, Eshghi O, Schreuder TH, Heijboer RJ, Keizer K, Tielbeek AV, den Hertog HM, Gerrits DG, van den Berg-Vos RM, Karas GB, Steyerberg EW, Flach HZ, Marquering HA, Sprengers ME, Jenniskens SF, Beenen LF, van den Berg R, Koudstaal PJ, van Zwam WH, Roos YB, van der Lugt A, van Oostenbrugge RJ, Majoie CB, Dippel DW; MR CLEAN Investigators. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015;372: 11-20.
- Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, Roy D, Jovin TG, Willinsky RA, Sapkota BL, Dowlatshahi D, Frei DF, Kamal NR, Montanera WJ, Poppe AY, Ryckborst KJ, Silver FL, Shuaib A, Tampieri D, Williams D, Bang OY, Baxter BW, Burns PA, Choe H, Heo JH, Holmstedt CA, Jankowitz B, Kelly M, Linares G, Mandzia JL, Shankar J, Sohn SI, Swartz RH, Barber PA, Coutts SB, Smith EE, Morrish WF, Weill A, Subramaniam S, Mitha AP, Wong JH, Lowerison MW, Sajobi TT, Hill MD; ESCAPE Trial Investigators. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015;372: 1019-1030.
- Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, Yan B, Dowling RJ, Parsons MW, Oxley TJ, Wu TY, Brooks M, Simpson MA, Miteff F, Levi CR, Krause M, Harrington TJ, Faulder KC, Steinfort BS, Priglinger M, Ang T, Scroop R, Barber PA, McGuinness B, Wijeratne T, Phan TG, Chong W, Chandra RV, Bladin CF, Badve M, Rice H, de Villiers L, Ma H, Desmond PM, Donnan GA, Davis SM; EXTEND-IA Investigators. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015;372: 1009-1018.
- Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, Albers GW, Cognard C, Cohen DJ, Hacke W, Jansen O, Jovin TG, Mattle HP, Nogueira RG, Siddiqui AH, Yavagal DR, Baxter BW, Devlin TG, Lopes DK, Reddy VK, du Mesnil de Rochemont R, Singer OC, Jahan R; SWIFT PRIME Investigators. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 2015;372: 2285-2295.
- Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, San Román L, Serena J, Abilleira S, Ribó M, Millán M, Urra X, Cardona P, López-Cancio E, Tomasello A, Castaño C, Blasco J, Aja L, Dorado L, Quesada H, Rubiera M, Hernandez-Pérez M, Goyal M, Demchuk AM, von Kummer R, Gallofré M, Dávalos A; REVASCAT Trial Investigators. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 2015;372: 2296-306.
- Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, Dávalos A, Majoie CB, van der Lugt A, de Miquel MA, Donnan GA, Roos YB, Bonafe A, Jahan R, Diener HC, van den Berg LA, Levy EI, Berkhemer OA, Pereira VM, Rempel J, Millán M, Davis SM, Roy D, Thornton J, Román LS, Ribó M, Beumer D, Stouch B, Brown S, Campbell BC, van Oostenbrugge RJ, Saver JL, Hill MD, Jovin TG; HERMES collaborators. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723-1731.
List of abbreviations:
NINDS trial: National Institute of Neurological Disorders and Stroke
ECASS III: European Cooperative Acute Stroke Study III