Health x Wellness
Should you be worried about IPF?
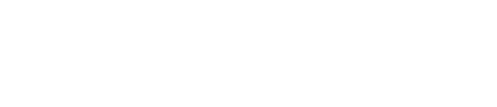
The Idiopathic pulmonary fibrosis (IPF) World Week recently ended on 24 September. IPF is a serious form of lung disease and impacts mainly middle-aged to older persons. Symptoms and diagnosis are ofttimes confused with pneumonia. The disease leads to “…restricted ventilation, impaired gas exchange, respiratory symptoms and exercise limitation, poor quality of life, and ultimately death.” Unfortunately, available treatment seems to only slow the progress of the disease and not cure it.
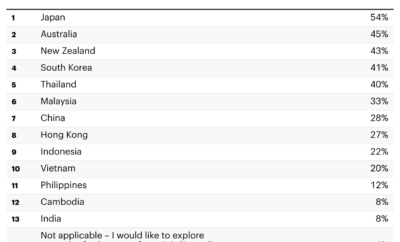
According to estimates, there are approximately 3 million people worldwide with IPF. However, given our ageing Asian population, the growing population of persons at risk and the incidence rate might increase. IPF is difficult to diagnose with many of the milder symptoms being associated with the process of growing older.
We speak with Professor Philip Eng, Senior Consultant, Respiratory & ICU Medicine at Mount Elizabeth Medical Centre, Singapore about IPF and why we should be more vigilant in understanding the disease.
Active Age (AA): What is Idiopathic Pulmonary Fibrosis (IPF)?
Professor Philip Eng (PE): Idiopathic pulmonary fibrosis (IPF) is a life-threatening condition where the lungs become thickened, stiff, and scarred over a period of time. The lungs then progressively lose their ability to take in and transfer oxygen into the bloodstream, decreasing the amount of oxygen the lungs can supply to major organs of the body. Although survival rates vary by patient, median survival after IPF diagnosis is two to three years in many studies all over the world.
AA: What are the signs and symptoms and when should people be worried enough to see a doctor?
PE: Symptoms of IPF include breathlessness, dry and persistent coughing which goes on for months. Clinical examination shows clubbing (widening and rounding) of the tips of fingers and toes, and sometimes weight loss if the disease is severe. Those who have persistent symptoms like shortness of breath or cough should go for medical evaluation, rather than attribute it to normal symptoms of ageing.
AA: What are the environmental and external triggers of IPF?
PE: IPF is defined as an idiopathic disease (i.e. of unknown cause).
AA: What should persons suspecting IPF share with their doctors for an accurate diagnosis?
PE: Before a diagnosis of IPF is made, certain other factors that can cause a similar disease must be excluded. For example, environmental toxins, drugs and other autoimmune diseases such as SLE. The patient may undergo certain blood tests and a CT Scan of the lungs called HRCT to make a confident diagnosis. Breathing tests and exercise tests help stratify the severity of the illness.
Patients suspected of having IPF should share with their doctors whether they are or were smokers, and how long they have been experiencing their symptoms. They should also try to recall what drugs they have been taking and whether they have been exposed to any environmental toxins.
AA: What are the treatments for IPF and how can a patient optimise their environment for treatment?
PE: As patients get progressively more short of breath with time, they will need long-term oxygen therapy. If eligible, they may need lung transplantation. Two new drugs have been recently approved for the treatment of IPF – Pirfenidone and Nintenanib. Studies have shown them to be effective in slowing down the decline of lung function.
For more information about IPF, readers can refer to the free e-book Life with IPF.