Health x Wellness
What is a knee replacement and what are my options?
A Q&A about knee replacement, options for surgery and what are some factors that lead to a diagnosis for the condition.
It is estimated that 20,000 Singaporeans undergo total knee replacement surgery every year and 96 percent of such replacements are caused by osteoarthritis.
This number is projected to grow, taking reference from projections that the demand for primary total knee replacements would increase by over 600 percent in the US compared to a decade ago.
Some major concerns amongst patients requiring knee replacements are loss of bone and cartilage, post-operative pain and complications, scarring, long recovery period before resuming normal daily activities, mortality risks and functional outcomes.
The Active Age discusses knee replacements with Dr James Wee, Medical Director & Consultant Orthopaedic Surgeon at Oxford Orthopaedics.
The Active Age (AA): Are knee replacements safe and how would it affect normal daily activities post-operation?
Dr. James Wee (JW): Knee replacement is very common locally, and most people would know someone who has undergone knee replacement. Although it is considered a major surgery, knee replacement is generally safe and the vast majority of patients do well after surgery, with success rates of up to 90 percent.
After they have recovered from the operation, patients can expect to have drastic reduction of their knee pain. They will also benefit from improved knee stability, reduced swelling and enhanced range of movement.
All these benefits will allow them to return to their daily activities, such as shopping, buying groceries, doing housework, meeting up with relatives and friends, and going on holidays (after the pandemic, of course!). Many are also able to return to recreational sports.
Knee replacement surgery returns independence to our patients, improves their general health and restores their quality of life.
Conventional wisdom dictates that knee replacements can last for only 10 years. With modern technology and improvements in surgical technique, patients can now expect much better.
Overall, big data (involving millions of patients) shows that more than 90 percent of total knee replacements (TKR) are still functioning at 15 years after surgery. Data from the Australian registry (which tracks all knee replacements in the country) shows that in patients with Osteoarthritis (OA), 91 percent of total knee replacements are functional at 19 years after surgery.
To summarise, we can expect less than 10 percent of patients to have failed knee replacements at 15 years!
Lastly, knee replacement surgery involves removing the damaged areas of the knee joint and replacing these areas with implants. Once these areas have been replaced, OA cannot recur, although the implants can wear out over time, as discussed above.
AA: What are the ways to achieve shorter scar, shorter hospital stay, quicker recovery and greater stability for knee replacement patients?
JW: We achieve this using Minimally-Invasive Surgical (MIS) techniques, which use smaller incisions and cause less injury to the soft tissues (such as muscles, tendons and ligaments) during the surgery. By using smaller incisions and causing minimal soft tissue injury, patients benefit from less pain, earlier discharge and much more rapid recovery and return to work.
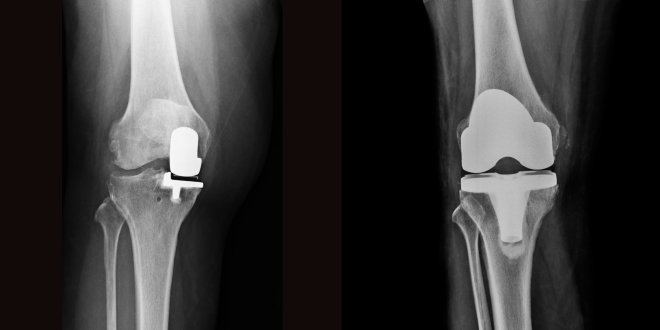
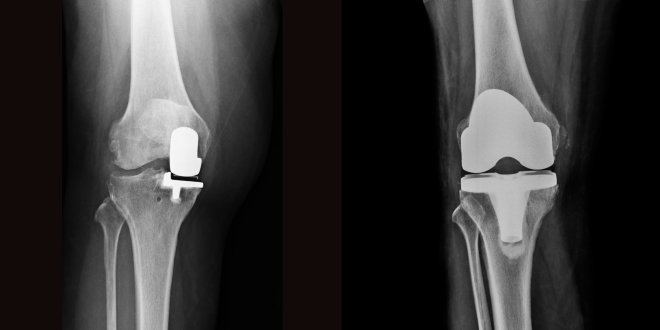
Partial knee replacement is particularly suited to MIS surgery, as only the damaged part of the knee has to be accessed during the operation (permitting a much smaller incision), and the partial knee replacement implants are much smaller than total knee replacement implants (only 30-40 percent the size of TKR implants). The image below shows a partial knee replacement on the left, and a total knee replacement on the right, illustrating the much smaller size of partial knee implants.
Hence, if the desired outcome is for a shorter scar, reduced hospital stay, faster recovery, and a more flexible and functional knee, then partial knee replacement surgery is the way to go!
The caveat is that for optimal results to be achieved, it is imperative that only suitable patients are selected (i.e. those with localised OA) and the operation is performed by an experienced partial knee replacement surgeon.
Partial knee replacement is suitable for most middle-aged and elderly patients afflicted with localised knee arthritis. Younger patients benefit from less post-operative pain, better scar cosmesis, faster recovery, a more natural and flexible knee, and a more rapid return to productive work and sporting activities compared to TKR.
Elderly patients, on the other hand, are exposed to less surgical risk with lower mortality and complication rates, and benefit from earlier discharge and swifter return to independent walking compared to their peers undergoing TKR.
In conjunction with MIS partial knee replacement techniques, there has also been a shift towards using Early Recovery After Surgery (ERAS) principles to help reduce pain and promote faster recovery. ERAS involves a multidisciplinary team comprising like-minded surgeons, anaesthetists, nurses and physiotherapists who work together synergistically to help patients recover better and return home sooner after knee replacement surgery.
AA: Must all patients with osteoarthritis go for total knee replacement or are other options available?
JW: OA occurs due to wear and tear in the knee over time, and the underlying problem is damage and loss of cartilage in the knee.
The typical candidate for knee replacement surgery would be someone with knee osteoarthritis who is experiencing significant knee pain that is affecting his/her daily activities, work, sports and leisure pursuits. The patient may also notice increasing knee stiffness and even “bow-legged” or “knocked-knee” deformities.
As knee replacement is for patients with relatively severe symptoms, it is not the first-line treatment for the majority of patients who have milder symptoms. In these patients with less severe OA, I generally recommend the following:
- A trial of physiotherapy for 3 to 6 months to strengthen the muscles around the knee, which can reduce knee pain and improve their ability to walk longer distances.
- Activity modification is useful to reduce the stress on the knees, and I advise my patients to avoid heavy loads, high impact activities like running and jumping, deep squats and excessive stair climbing.
- Diet and weight loss is also useful to reduce the stress on the knees.
- Anti-inflammatory and painkiller medications can be useful to manage knee pain in the short term, especially if there are periodic episodes of pain flare-ups.
- Knee braces, mainly during strenuous activities, can help reduce pain and swelling, and improve walking distances. Supportive shoe insoles can also be helpful.
In patients with significant pain from knee OA that has not responded to physiotherapy and other non-surgical methods, knee replacement surgery is the gold standard treatment.
However, if the patient is not willing to go for knee replacement surgery, injections into the knee joint can help. Knee joint injections, such as steroids or lubricants (also called viscosupplementation injections), can help reduce knee pain in patients with OA. Steroid injections typically last approximately 3 months, while lubricant / viscosupplementation injections can last for 6 to 12 months on average. However, these injections do not work for every patient, and some patients see no improvement in symptoms, or experience early pain recurrence.
Another alternative to knee replacement surgery is “keyhole” surgery (also called knee arthroscopy). This is a relatively minor procedure that can be done in the day surgery setting and has the advantages of being low risk and allowing early recovery. However, “keyhole” surgery is only suitable for patients who have knee pain attributable to a localised cause such as a meniscus tear or a loose body. For patients with diffuse and severe OA of the knee, “keyhole” surgery is often less successful.
Lastly, in very young patients (30s and 40s) with localised knee arthritis, knee osteotomy can be an option that preserves the native joint. In knee osteotomies, the tibia and/or femur is broken and fixed with metal plates and screws to change the shape of the knee joint, redirecting the weight-bearing forces away from the localised area of arthritis toward healthier areas of the knee. Knee osteotomy can potentially reduce knee symptoms in young patients, but is associated with more post-operative pain, higher complication rates and is often shorter-lasting than knee replacement.
When the abovementioned options fail to provide good relief for knee pain, then knee replacement surgery becomes the best treatment modality. There are two options when it comes to knee replacement surgery – conventional total knee replacement, where the entire knee joint is replaced with a prosthesis, and partial knee replacement, which is a targeted treatment that replaces only the damaged compartment of the knee and preserves the healthy areas.
AA: Is partial knee replacement safer and more effective than total knee replacement?
JW: TKR typically involves replacing the entire knee joint with a prosthesis. In many cases, this results in healthy and functional areas of the knee joint being removed to accommodate the TKR implants, which occupy the entire knee joint. The advantage of TKR is that the operation is generally more straightforward to perform and can be done for virtually all patients with severe knee OA.
In recent years, the thinking amongst many knee surgeons has shifted to prioritise a more targeted approach to preserve healthy areas of the knee joint. In many patients with severe OA symptoms, the knee damage starts out localised to a particular area or compartment of the knee joint, typically the inner side of the knee (medial compartment) in ~90 percent of patients. This is particularly true of patients who seek treatment early before the joint damage has spread to the other knee compartments – the outer side of the knee (lateral compartment) and the knee cap (patellofemoral compartment).

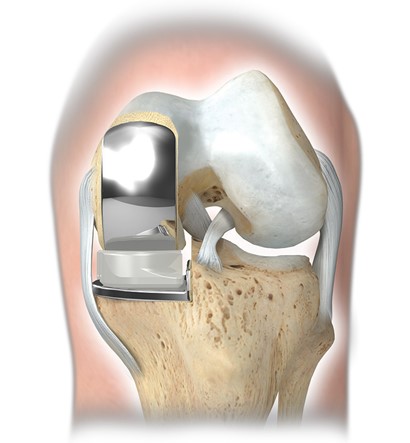
In patients with only localised knee damage, it is unnecessary and wasteful to remove the areas of healthy cartilage, bone and ligaments just to accommodate a TKR implant. Indeed, patients with only localised knee damage are ideal candidates for partial knee replacement (also called unicompartmental knee arthroplasty or UKA). In partial knee replacement, only the damaged compartment of the knee joint is removed and replaced by an implant. Consequently, as much as 60-70 percent of the patient’s native knee is preserved after partial knee replacement surgery; also, all the major knee ligaments are preserved (whereas some ligaments are sacrificed in TKR).
Many knee surgeons today understand the benefits of preserving the healthy parts of the knee; after all, the knee we were born with is still the best knee we can have!

Partial knee replacement has numerous clinical advantages over conventional TKR.
First, it is well-established by large studies that partial knee replacement is safer than TKR and has lower major complication and mortality rates, both during and after surgery. Hence, it is suitable for many older patients with concurrent medical problems such as heart conditions, previous strokes and diabetes who would otherwise be at significantly higher risk for TKR surgery.
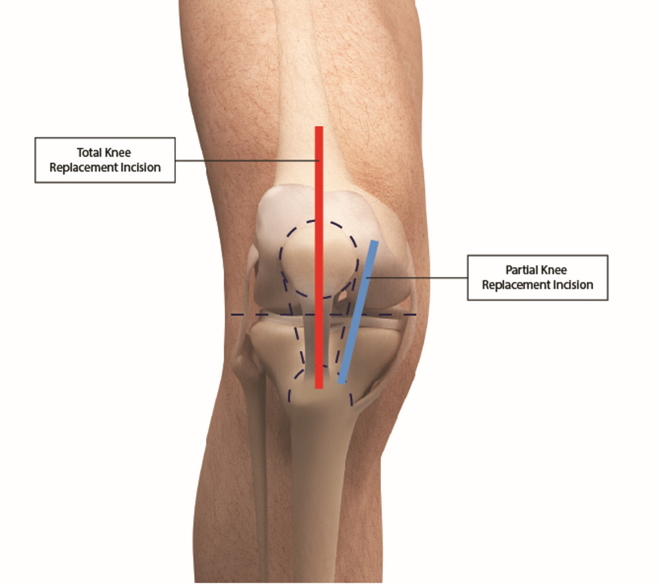
Second, partial knee replacement can be done using minimally invasive surgical (MIS) techniques, and the skin incision required is approximately half the length compared to TKR (see diagram below). In addition to the cosmetic advantage of a far shorter scar, the other benefit of UKA is far less injury to the joint and soft tissues during the procedure, and patients have significantly less pain after surgery compared to TKR. This leads to more rapid recovery, almost immediate return to walking on the day of surgery itself, and early discharge home. In fact, at the hospital I worked previously, I led a team that pioneered early and safe discharge home within a day after partial knee replacement surgery. The patients were able to save money and benefit from recovering in the comfort of their own homes – they were very happy!
Third, by preserving more than half of their native knee joints, partial knee replacement is associated with significantly better knee movement than TKR. This is particularly beneficial for patients who have to kneel or squat at work or for religious reasons.
Fourth, patients who undergo partial knee replacement usually report a more natural-feeling knee compared to their peers who underwent TKR, owing to the knee-preservation approach. Compared to TKR patients, they typically have better recovery and higher functional levels in the early stages after surgery.
Finally, in the event that the partial knee implant is worn out and needs to be revised after many years, the subsequent operation is typically straightforward and involves conversion to a standard total knee replacement, usually with excellent outcomes. On the other hand, if a TKR implant fails and has to be revised, the operation required is usually bigger and more complex, involving larger and more costly specialised implants.
In summary, partial knee replacement is safer than TKR, involves a smaller scar, and is more effective in returning patients to early walking and activities. Patients also experience far less pain and are able to return home sooner after surgery, often within a day. They benefit from a more natural-feeling knee and better knee bending & flexibility. In the long term, a partial knee replacement performed by an experienced knee surgeon has been shown by many studies to be as lasting and durable as a total knee replacement. Furthermore, in the event that a partial knee replacement fails after many years of service, the revision operation is more straightforward and less risky than after a failed TKR.
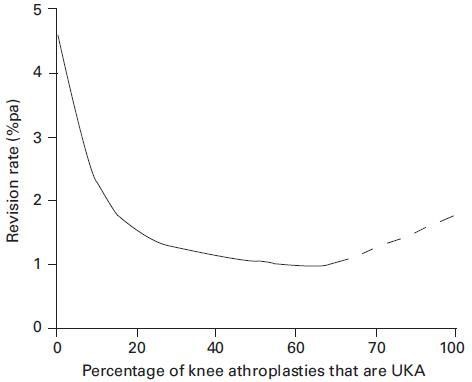
The main drawbacks of partial knee replacement are twofold. Firstly, only patients with localised arthritis of the knee are suitable; patients who seek treatment late with severe generalised OA, as well as patients with inflammatory arthritis like gout and rheumatoid arthritis, are not good candidates and should undergo TKR instead. Secondly, partial knee replacement surgery is more technically demanding to perform than TKR, and studies have shown that knee surgeons require further subspecialised training and significant experience in partial knee replacement surgery to deliver consistently good results. Research from the UK shows that complication rates are significantly lower for knee surgeons whose partial knee replacement workload comprises at least 20% of all their knee replacement surgeries (see graph below).
The take-home message is this – it is important to seek medical attention early if you have knee pain before the knee damage becomes too widespread, and consult an experienced and trained partial knee replacement surgeon to assess if you are suitable.
AA: What is the latest treatment modality – the Oxford partial knee replacement about?
JW: The Oxford partial knee replacement system has been growing in popularity in recent years as knee surgeons increasingly recognise the advantages of partial knee replacements. The Oxford partial knee replacement has undergone continuous refinement for approximately 40 years. Apart from having a long track record, it also has the distinction of being the most clinically researched and proven partial knee replacement system currently available, having been developed and studied by generations of surgeons at Oxford University Hospitals.
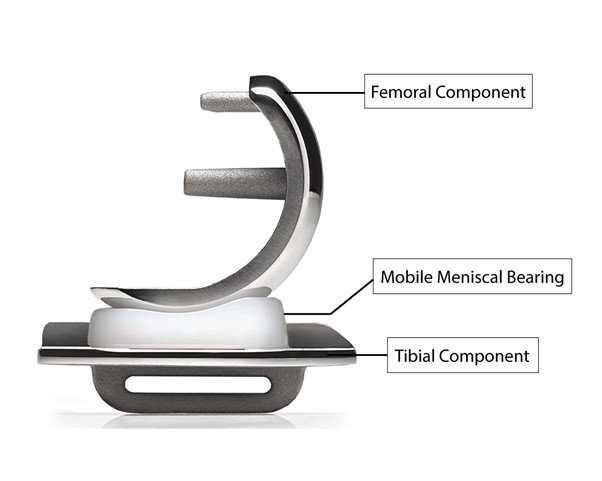
All knee replacement implant systems comprise 2 metal components (1 on the femur and 1 on the tibia), with a specially fabricated plastic (polyethylene) bearing in between the metal components for lubrication. In the case of the Oxford partial knee replacement, the plastic bearing is not fixed to either metal component; instead, it is allowed to glide freely between the metal components. This mobile-bearing design of the Oxford partial knee system reduces the stresses and wear rate of the plastic bearing, and may also provide a more natural feel to the knee, compared to designs where the plastic bearing is fixed to a metal component (fixed-bearing designs).
A key reason that the Oxford partial knee system has become established as one of the top partial knee replacement implants worldwide (and is recognised as the top mobile-bearing partial knee system) lies in its research pedigree. The Oxford partial knee replacement system has the most extensive clinical data amongst the various partial knee systems, and this data has been validated by multiple research centres in the US, Europe and Asia. This comprehensive data set is specific to the Oxford partial knee system, and allows surgeons to have a clear understanding of: which patients are most appropriate, the types of knee problems that can be effectively treated, and how to best achieve optimal outcomes in diverse patient groups.
The Oxford partial knee system is renowned for being the most clinically proven partial knee replacement available.
Another reason for the success of the Oxford partial knee lies in the continuous efforts and innovations over 40 years to improve its accuracy and ease of use, which has produced successively better generations of implants. In its latest version, the Oxford partial knee system is optimised for minimally-invasive surgical (MIS) techniques, and has been clinically proven to achieve reliable and accurate implant positioning, with improved knee stability and flexibility compared to other conventional partial knee systems.
Implant innovation has also led to the development of the cementless Oxford partial knee implant. The large majority of knee implants require a special bone cement for fixation to bone, and the downside to this is that the cement can be worn out over time, leading to implant loosening. For the cementless Oxford partial knee implant, the implant surface is specially designed to promote rapid ingrowth of the patient’s bone – hence the implant is held firmly in place by living bone, which solves the problem of cement wear and loosening. The UK and Australian knee registries have both validated this concept, showing that cementless partial knee implants are significantly better-lasting than cemented implants at 15 years after surgery and beyond.
In Singapore, the Oxford partial knee system is the only cementless partial knee replacement implant currently available.

AA: What are some of the factors – environmental or otherwise – that lead towards a diagnosis or recommendation of knee replacement?
JW: OA, which occurs due to wear and tear, is by far the most common reason for knee replacement surgery. Other groups of patients who may need knee replacement include those who have:
- Inflammatory joint diseases such as rheumatoid arthritis and gout; such diseases usually affect the entire knee joint (i.e. generalised damage)
- Old sports injuries such as a ruptured knee ligament, a torn meniscus (a cartilage-like structure in the knee that acts as a shock absorber), or localised cartilage damage (also called osteochondral injury).
- Previous accidents causing fractures to the bones around the knee (femur and tibia)
- Disruption of the blood supply to the bones around the knee (also called osteonecrosis) causing damage to the knee cartilage
- Uncommon conditions such as previous knee joint infections and tumours around the knee
A trend that many of my colleagues and I have observed in the past few years is that patients are coming to us with severely symptomatic knee OA at a younger age, and there is a significant group of patients in their early to mid-50s who already require knee replacement surgery.
We attribute this to a few reasons. Firstly, patients are much more active nowadays, and engage in sports and strenuous activities well into their 40s, 50s, and beyond. These patients place higher demands on their knees and wear them out sooner. Secondly, many middle-aged patients carry sports injuries from their youth, and these knee injuries hasten the progression of knee OA. Thirdly, patients are more aware and well-informed these days, and they know that outcomes are better if they seek early treatment for knee injuries and pain.
For this group of relatively young patients in their late 40s and 50s who suffer from severe knee OA symptoms, the cartilage damage is often localised to a single compartment of the knee initially. Hence partial knee replacement is a particularly attractive alternative to conventional TKR in this younger patient group. Partial knee replacement has the advantages of less post-operative pain, faster recovery, and much earlier return to productive work and sports activities, which is especially important to this group of patients who are still in their peak working years and are still physically active.
AA: What are the disadvantages associated with opting not to do a knee replacement whether full or partial?
JW: Knee replacement is a surgical procedure whose principal aims are to relieve knee pain, restore knee function, and return patients to activity and a better quality of life. By improving function and activity levels, knee replacement also promotes better general health and fitness in patients who successfully undergo surgery.
Patients are happier and enjoy a better quality of life because they are more able to partake in sports and participate in recreational activities such as going on holidays overseas and meeting up with friends and family.
Conversely, patients who have severe symptomatic knee arthritis who opt against knee replacement surgery typically find themselves trapped in an increasingly sedentary lifestyle, confined by the pain and stiffness in their knees. Over time, many of these patients end up being homebound or restricted to using mobility aids such as wheelchairs. This has severe repercussions on their cardiovascular fitness and general health, and can potentially put them on the back foot when it comes to heart attacks and strokes. Prolonged immobility also puts them at risk of complications such as chest infections (pneumonia), urinary tract infections, pressure sores, deep vein thrombosis (blood clots forming in the legs) and pulmonary embolism, which can be life-threatening.
Hence, in patients who have persistent or worsening knee pain, it is important to seek medical advice early. Early diagnosis and treatment of knee osteoarthritis is important in achieving optimal outcomes, earlier return to work and sports, and better quality of life.
Image credit: Oxford Orthopaedics and Photo by Lucaxx Freire on Unsplash